Sleep and Autism
TOP TIPS FOR BETTER SLEEP

What is sleep and why is it important?
Although it can appear a passive activity, when we sleep, our brain is in fact highly active. Sleep is complex process made up of several different stages, during some we sleep very deeply, whereas others are lighter, meaning we could be woken more easily. While we sleep, our brains carry out essential biological processes. Although these processes are still not fully understood, we know that sleep;
- Is good for our physical health. It strengthens our immune system, helping us to fight off illness. Essential growth hormones are also released during sleep.
- Is good for learning and development. Sleep supports memory and concentration.
- Is good for the emotional wellbeing of the whole family. You don’t need us to tell you this! During sleep the brain makes sense of the day’s events, improving mood and emotional well-being. A tired child has less ability to regulate and express themselves, so they would appear to be more hyperactive and disruptive. A tired parent has lower level of patience and higher level of frustration.
Although sleep forms a part of our day naturally, for children to learn to sleep at set times, in set places, following certain rules (or expectation from parents) is something parents have to teach them and support them to achieve.
You are not alone!
Sleep problems are common! Amongst young children aged 2 to 5 years, up to half may experience sleep problems (Shakankiry 2011, Cheng et al. 2021). However, such problems are significantly more common in autistic children of this age, compared to children of the same age without a diagnosis (Reynolds et al., 2019) . Overall, between 50 and 80% of autistic children experience sleep problems (Rana et al. 2021) . Autistic children tend to sleep less at night overall and wake more often, with these differences most marked in preschool children (Humphreys et al., 2014).
How much sleep does my child need?
Here are average times most child need to sleep according to the National Sleep Foundation. You will notice there is a big range in what is needed depending on the individual child.
| Age | Recommended Total Sleep | May Be Appropriate |
|---|---|---|
| Toddlers (1 to 2 years old) | 11 to 14 hours | 9 to 16 hours |
| Pre-schoolers (3 to 5 years) | 10 to 13 hours | 8 to 14 hours |
After 3 years, gradually reduce then stop daytime naps.
Before you start – key points to remember
- Your child can learn to sleep better but it takes time.
- Start with small changes but then stick to the change you have made.
- BE CONSISTENT!
Where to Start?
Preparation is half the battle. Here are some things to consider to encourage good sleep habits. Making sure you have these basics in place is a great first step towards improvements in sleep.

| 1. Preparing the environment for sleep: |
|---|
| Room temperature for sleeping is important. Ideal is 16 to 20 degrees centigrade. |
| Reduce light. Use blackout blinds, turn hallway lights off and use a small red bulb in a bedside lamp if necessary. |
| The bed and bedding are important. Ensure the bed is comfortable. Tucked in duvets and/or a weighted blanket can assist. |
| Reduce noise or use a ‘masking device for white noise’. Also reduce other noise in the home such as from the TV or playing noises from other children. |
| Reduce your child’s access to toys in the bedroom during bedtime. Put stimulating toys in a basket/ laundry basket and remove it from the child’s room; a few cuddly toys could be left for comfort. |

| 2. Preparing your child for sleep |
|---|
| No screens at least an hour before bedtime. Their blue light is too stimulating. |
| It’s best NOT to sleep on a full stomach, no food and drink at least an hour before bedtime. |
| Ideally eliminate caffeine from midday. Fizzy drinks often have caffeine as does tea and chocolate. |
| Ensure your child has enough water to drink at least an hour before bedtime. This gives them a chance to empty their bladder before they sleep, reducing the chance of bedwetting, or waking others for help to go to the loo. |
| Calcium based food or drink can help promote sleep, but not too near bedtime. |
| Exercise e.g. cycling, running, playing in the park has to be finished at least 2 hours before bedtime. |
| Introduce and stick to a clear and consistent bedtime routine. You can use a visual schedule to help your child understand and follow this. See more information below. |
| A quiet squash or squeeze can be relaxing for many autistic children. This can help them wind down for sleep if included as part of the bedtime routine. You can find out more about this on our advice page on Sensory Regulation and Participation. |
If you would like to download a copy of this checklist with visual support to stick on your fridge for your own use, please click here.
Developing a bedtime routine
- It is essential to repeat the bedtime routine in the same order and at the same time each night, including at weekends and during the holidays. This will strengthen your child’s body clock and help them understand that it is time to sleep.
- Choose your child’s bedtime carefully, working back from the time you want your child to wake.
- Your child should be put in the place where they will sleep awake, rather than being lifted into place from somewhere else once asleep.
- Some autistic children may find bath time stressful. Eliminate bathing near bedtime if this is stressful for your child and instead do this earlier in the day as needed. If it is a happy event, finish bath time about half an hour before bedtime to allow your child’s body temperature time to settle.
- You can keep a few things specifically for bedtime, such as a special toy, a blanket or soft music. Keeping these for bedtime only will help your child link them to sleep and prompt them to settle when they see them.
- After saying goodnight, try to use little language, no eye contact and a set phrase, which you repeat, such as “…Sleep time…”
Example bedtime routine with timings
Here is a possible schedule for your bedtime routine. This is just an example and will be unique to every family depending on your own family culture. The important thing from the point of view of encouraging sleep is that the final part of the routine is kept short.
| Time | Activity |
|---|---|
| 5.30pm | Child has meal |
| 6.00pm | Free play |
| 7.00pm | Quiet play and calming activities, such as jigsaws, building and colouring. No computer games or television from this point on. |
| 7.30pm | Revisit your bedtime social story or visual schedule if needed (see below). Child goes to the toilet and then bath time. |
| 7.40pm | Child in pyjamas with teeth cleaned, child is ready for bed. |
| 7.45pm | Child into bed, bedtime story/ cuddles. |
| 7.59pm | Parent says goodnight. |
| 8.00pm | Lights out & leave child to settle. |
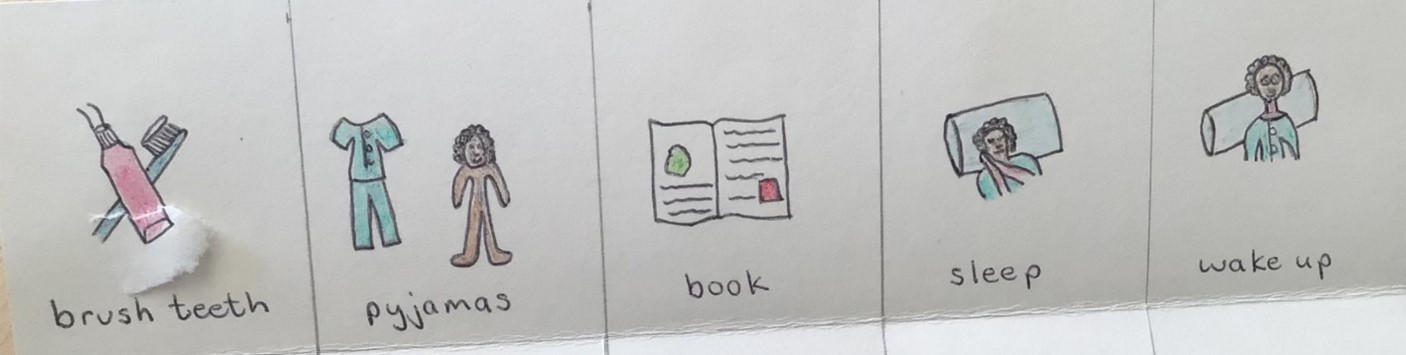
A Visual Schedule
A social story or visual schedule can help your child understand and follow expectations. You can make your own with real pictures of your family or just draw something simple like this. You can click here to download some images you may wish to use to create you own.
What next?
- Watch our sleep advice video. If you have implemented these strategies and are still having difficulties with your child’s sleep, watch our team’s video on sleep for further advice (the links for these should have been shared with you following your child’s diagnosis). The video has ideas to help you teach your child to settle without you and then to sleep in a bed alone.
- Keep and sleep diary. We recommend you keep a record of your child’s sleep over the course of a week, as this will help you, and the team to understand your child’s needs better. Click here to download a copy of a sleep diary together with an example. Keep this by your bed so you can fill it in immediately. If you wait, it will be hard to remember. Always answer honestly – remember there is no shame in your child having sleep difficulties and you are not alone in struggling with this!
- Book an individual support session. Once you have watched the video and completed a two-week diary of your child's sleep, please return the completed sleep diary to the team at this email address: whh-tr.islingtonsct@nhs.net. Once we receive your completed diary, we will contact you to book an appointment for you to discuss your questions and queries with a member of our team.
- You can also access further advice from the National Autistic Society.
Last updated10 Sep 2025